Anthony Karabanow, MD
In a poor country such as Haiti, early disease identification and management is essential. Haitians have no access to unemployment or disability financial support. There is no rehabilitation or long term care facilities in Haiti. Home health care is non-existent. There are no public measures in place to accommodate disability. Thus, at a certain burden of disease, survival in Haiti becomes impossible. The most effective medical intervention strategy in Haiti is to intervene early in the course of disease to assure the patient a high level of function and a minimal need for costly, frequent and potentially unavailable medical care.
Diabetes is a perfect example of this concept. Under optimal conditions, diabetes is managed by routine medical visits where scrupulous attention is payed to blood sugar control and the control of other associated cardiovascular comorbidities. Under worst case conditions, this disease ravages the body resulting in heart disease, stroke, limb amputation, kidney failure and blindness. In a country ill-suited to manage such advanced disease (both medically and socially,), we must aggressively pursue prevention and early case identification/treatment. This requires an investment in public health and primary care.
A 2006 study by FHADIMAC (Fondation Haïtienne de Diabète et de Maladies Cardio-vasculaires) identified a prevalence for diabetes of 4.8% in men and 8.9% in women amongst a sample of Haitians living in Port-au-Prince1. WHO data indicates that 90% of diabetics are type II (i.e. adult onset, typically non-insulin dependent). Of interest, more than 80% of people with diabetes live in low/medium income countries.
 Diabetes is defined as persistently elevated blood sugars. This results from either an absolute or relative insulin deficiency. In type 1 diabetes, the pancreas undergoes an autoimmune attack which renders it incapable of insulin production (absolute insulin deficiency.) This typically occurs in younger people. They have a life-long need for insulin administration. In type 2 diabetes, insulin production is relatively inadequate compared to blood sugar levels. This usually occurs in adults, has a genetic component and correlates with obesity. Type 2 diabetics can often be controlled with diet and oral medications. At times, these patients may require insulin as well.
Diabetes is defined as persistently elevated blood sugars. This results from either an absolute or relative insulin deficiency. In type 1 diabetes, the pancreas undergoes an autoimmune attack which renders it incapable of insulin production (absolute insulin deficiency.) This typically occurs in younger people. They have a life-long need for insulin administration. In type 2 diabetes, insulin production is relatively inadequate compared to blood sugar levels. This usually occurs in adults, has a genetic component and correlates with obesity. Type 2 diabetics can often be controlled with diet and oral medications. At times, these patients may require insulin as well.
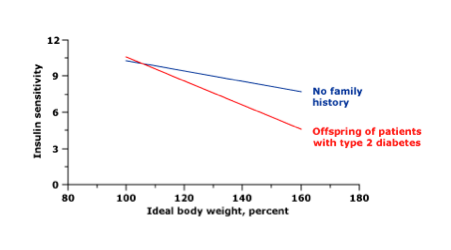
The interplay between genetics and obesity in the development of type 2 diabetes is well illustrated in an article by Kahn in Diabetes 19942. Kahn determined insulin sensitivity in patients with genetic risk of diabetes versus that in control subjects. At normal body weight, both groups demonstrated equivalent insulin sensitivity. However, as body weight increased, those with genetic risk showed decreased insulin sensitivity compared to controls. In other words, those with a genetic tendency to diabetes are more likely to develop diabetes as they become obese.
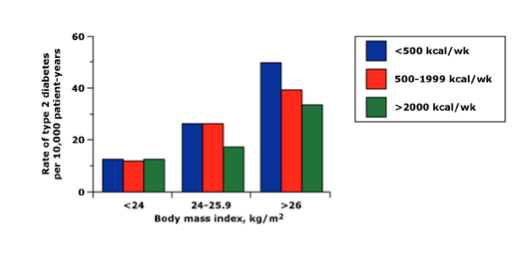 The relationship between body weight, exercise and diabetes was also evaluated in a New England Journal of Medicine article in 1991 by Helmrich et al3. Diabetes rates correlated with obesity while exercise was protective against diabetes.
The relationship between body weight, exercise and diabetes was also evaluated in a New England Journal of Medicine article in 1991 by Helmrich et al3. Diabetes rates correlated with obesity while exercise was protective against diabetes.
We commonly think of Haiti as a country ravaged by poverty and thus malnutrition. However, there are also surprising data on obesity in Haiti from the 2010 World Bank report “Promoting Nutrition Security In Haiti”4. Data on Haitian children show that 16.1% of children fall into the category of overweight.
Moreover, it has been established that low-birth weight children (due to maternal under nutrition) or who suffer nutritional deficiencies in early childhood are actually at higher risk of later developing obesity.
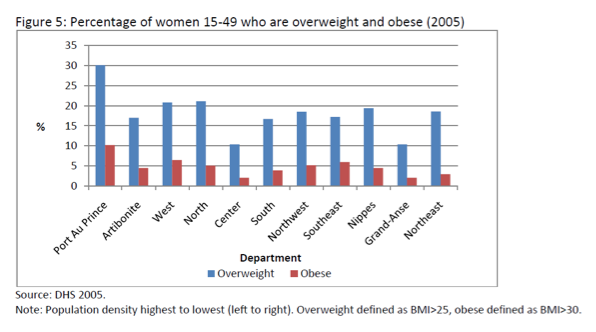 Obesity data in women is particularly of interest due the correlation between maternal obesity and child obesity.
Obesity data in women is particularly of interest due the correlation between maternal obesity and child obesity.
Type 1 diabetics are not commonly seen in Milot. This is most likely the result of premature death. Type 1 diabetics require insulin at all times. Without insulin, they rapidly develop a condition known as DKA (diabetic ketoacidosis.) This condition is characterized by elevated blood sugars, acid-base disturbance, electrolyte deficiencies and dehydration. Such cases were unfortunately described after the Haitian earthquake when type 1 diabetics were cut off from their supplies of insulin.
Both NPH (long acting) and regular insulin (short acting) are part of the Hôpital Sacré Coeur formulary.
Type 2 diabetics are commonly seen in Milot. Indeed, rates are expected to rise as Haitians become heavier and less active. There are 2 medications available to treat such patients in the Hôpital Sacré Coeur formulary – glyburide and metformin. The first causes increased secretion of insulin from the pancreas. The other reduces liver production of glucose and increases muscle tissue sensitivity to insulin.
Diabetics should be seen by a physician every 3 to 4 months for a routine visit. During such a visit, the physician will inquire as to any symptoms of heart disease, stroke, skin breakdown or vision loss. Blood pressure should be checked and the physical examination should include a meticulous foot exam. Diabetics are liable to develop peripheral neuropathy – i.e. the loss of sensation in their feet. This can lead to unnoticed skin breakdown and infection. The foot exam includes examination for such skin breakdown as well as for loss of sensation. Skin breakdown needs to be rapidly treated to avoid potential loss of limb. Loss of sensation requires the physician to advise the patient to avoid going barefoot and to examine his feet regularly.
All diabetics need dietary counseling. Adhering to a diabetic diet presents unique difficulties in Haiti where a carbohydrate rich diet is favored. Rice and fruit, in particular, are rich in carbohydrates. The following illustrates the high carbohydrate content of rice and fruit in terms of equivalent quantities of carbohydrates (15 grams:)
- 1 slice of bread
- 1/3 cup of cooked rice
- 1/2 cup of cooked dried beans
- ½ small mango or papaya
- 1 small banana
- 1/2 cup fruit juice
Typically, the equivalent carbohydrate content of 4 pieces of bread is permitted at each meal (60 grams). Alternatively, one can adhere to the “plate method” where ¼ of the plate is filled with meat, ¼ with starchy foods and ½ of the plate with vegetables. Green, leafy vegetables help provide satiety with minimal carbohydrate loading. Unfortunately, meat is relatively expensive and vegetables less commonly available than fruit.
Blood sugar control is difficult to gauge in Haiti. Patients do not have blood sugar meters for home use. Any single blood sugar value obtained in clinic is of little use. The HgA1c is the most valuable tool in the US for tracking blood sugar control. It provides a measure of average blood sugars for the previous three months. However, this is an expensive test and not currently available at Hôpital Sacré Coeur. Bringing the HgA1c into routine use at Hôpital Sacré Coeur would be a major step forward in the care of our diabetic patients.
Diabetics are already at high risk of heart and other vascular diseases. Thus, blood pressure and cholesterol control represent important elements of diabetes care. Blood pressure is easily measured in clinic. A cholesterol test is available from the lab. There are a number of blood pressure medications available on the Hôpital Sacré Coeur formulary: atenolol, HCTZ, amlodipine and quinapril. The last agent is particularly important for diabetics as this class of agents (ACE inhibitors) has been shown to reduce the rate of kidney injury. Cholesterol medication (“statin”) is also on formulary.
Diabetics are at high risk of vision loss as the disease attacks the blood vessels at the back of the eye. In the US, an annual ophthalmologic exam is recommended. HSC has access to visiting eye teams who may perform this function. Unfortunately, laser therapy to treat diabetic eye disease is still not available.
As Haiti strives to improve its care of diabetics, the following steps need to be taken:
1) Regular screening of adults to identify this disease at the earliest possible stage.
2) Routine access to diabetes education to emphasize appropriate dietary modification, weight loss and routine self care.
3) Routine follow-up to monitor blood sugar, blood pressure, cholesterol and developing cardiovascular disease.
4) Routine screening for diabetic foot disease.
5) The introduction of the HgA1c (preferably) or at least home blood sugar monitoring.
6) Uninterrupted access to diabetic, blood pressure and cholesterol medication.
Due to the importance of diabetes in Haiti, this topic was selected for the first educational symposium at Hôpital Sacré Coeur in January 2011.
References:
1. Jean-Baptiste,ED et al. Glucose intolerance and other cardiovascular risk factors in Haiti. Prevalence of Diabetes and Hypertension in Haiti. Diabetes Metab. 2006 Nov;32(5 Pt 1):443-51.
2. Kahn CR. Banting Lecture. Insulin action, diabetogenes, and the cause of type II diabetes. Diabetes 1994; 43:1066.
3. Helmrich SP et al. Physical activity and reduced occurrence of non-insulin dependent diabetes mellitus. N Engl J Med 1991; 325:147-152.
4. Promoting nutrion security in Haiti: An assessment of pre and post earthquake conditions and recommendations for the way forward. World Bank Report Sept 2010.









