Leptospirosis is known to be endemic in Haiti. The Haitian System of Sanitary Information reported between 6,500 and 11,000 cases of febrile jaundice annually between 2005 and 2008. More than 12,700 cases were reported between January and June 2009. A Haitian study from the early 1960’s reported that 30% of such infections were due to leptospirosis.1 A previous report indicated that 64.9% of transitional Haitian immigrants in Cuba had antibodies to leptospirosis (indicating prior infection2.)
Leptospirosis is caused by the spirochete Leptospira interrogans. Spirochetes are spiral shaped organisms that include the causative agent of syphilis. Leptospirosis is the most common zoonosis (infection acquired from animals) in the world. The organism infects a wide variety of animals including: dogs, pigs, cattle, horses, sheep and goats. Animals with this infection do not necessarily have to be symptomatic.
However, this infection can cause death in dogs and spontaneous abortions in cattle, pigs, sheep and goats. Infected animals shed the organism in their urine which results in contamination of water sources. The organism can remain viable in the environment for months.
 Leptospirosis infects humans through skin abrasions or via mucous membranes or conjunctiva. Rare cases have been acquired through contaminated food or via the aerosol route.
Leptospirosis infects humans through skin abrasions or via mucous membranes or conjunctiva. Rare cases have been acquired through contaminated food or via the aerosol route.
Sewer workers, outdoor and agricultural workers (e.g. sugarcane farmers) are particularly at risk.Outbreaks may occur after heavy rainfall or flooding.
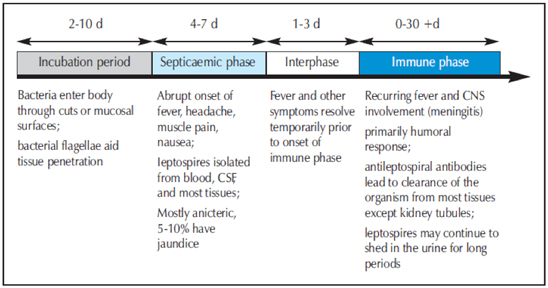
Of note, there are two clinical stages to this disease with a brief symptom free period between stages. The septicemic stage results from the widespread dissemination of the bacteria throughout the bloodstream and practically all organs and tissues. This stage consists of a non-specific flu-like illness (i.e. fever, chills, muscle pain and headache.) Patients often complain of muscle pain in the calves and lower back but this finding is far from diagnostic. Another potentially suggestive finding is a conjunctival suffusion (“red eye.”) The interphase is characterized by the resolution of fever and other symptoms. The immune phase results from the clearance of the organism by the immune system. This stage consists of recurring fever and often aseptic meningitis. However, there may also be organ specific syndromes such as: myocarditis, kidney failure, hemorrhage, respiratory failure, liver failure and uveitis. Death may occur due to multi-organ system failure. With severe disease, the stage-like nature of classic leptospirosis may not be apparent. The pathophysiology of severe disease is widespread damage to the endothelial lining of small blood vessels resulting in organ ischemia.
The diagnosis is usually made by serology (i.e. antibody detection.) However, this test is not routinely available in Haiti. Other suggestive (but non-specific) laboratory results include an elevated white count (with left shift), an abnormal urine analysis (proteinuria, pyuria,) elevated CK, and abnormal liver function tests (elevated transaminases, bilirubin.)
The treatment of leptospirosis is as follows:
• Outpatient adults: Doxycycline 100 mg PO BID
• Outpatient pregnant women and children < 8 yrs: amoxicillin
12.5 mg/kg PO TID
• Hospitalized adults: Ceftriaxone 1 GM IV Q 24 hrs
• Hospitalized children: Ceftriaxone 100 mg/kg IV Q 24 hrs
The duration of treatment is typically 7 days as there are multiple leptospirosis serovars (subtypes,) infection with one serovar provides no protection against infection with another.
Prevention of leptospirosis includes: protection of food/water from animal contamination, avoiding water run-off from farms, rodent control, avoiding stagnant water, the use of protective clothing and animal vaccination.
References:
1. Laroche, Victor, “La leptospirose en Haiti,” Bol Oficina Sanit Panam,” 1965; 59(5): 414-422.
2. Pupo, L. et al., “Leptospirosis: Informe serologico sobre la poblacion haitiana de transito en Cuba,” Rev Cubana Med Trop., 1983; 35(1): 112-118.
3. WHO South-East Asia Regional Office, “Leptospirosis Fact Sheet.”