 By Brisma Jean Pierre, MD
By Brisma Jean Pierre, MD
HSC Cardiologist and Master of Emergency Medicines, Head of HSC Emergency Department and Outpatient Clinic
Peripartum cardiomyopathy is a rare case of the deterioration in cardiac function, but in Haiti, it is a major health problem because the number of patients suffering from this disease progressively increases. This condition is one of the important causes of heart insufficiency in Haiti’s young women and results in very high mortality. The prevalence rate in Haiti is 1 case for every 350 to 400 pregnancies. [It is estimated that the incidence of PPCM in the United States is between 1 in 1300 to 4000 live births.]
Peripartum cardiomyopathy is defined by the presence of signs and symptoms of cardiac insufficiency that occurs during the last month of pregnancy until the fifth month after childbirth. In the absence of an obvious etiology and in the absence of any other known and preexisting heart disease, diagnosis is made thorough research. Symptoms include: dilation of the left ventricle (diameter end-diastolic > 2.7 cm/m²) and systolic dysfunction of the left ventricle (Ejection Fraction of the left ventricle < 45% or Fraction of shortening < 30%).
Peripartum cardiomyopathy is multifactorial. The risk factors for this disease are the age of the patient, with a higher risk factor for women over 30, low socioeconomic level, black race, multiparity, pregnacy of twins, and hot and humid climate. But in Haiti, there are also cases in patients who are less than 20 years old.
 While the exact cause of PPCM is unknown, reference has been made to the possible involvement of various pathophysiological avenues e.g. infections, cardiotropic viruses, autoimunity or immune system dysfunction; inflammatory, metabolic and endocrine triggers, genetics, pre-eclampsia, which can produce an achievement, functional and anatomical cardiomyocytes and finally progressive dilation of the heart chambers with systolic dysfunction (BADEA, Ann Fr year Reanim, 2009, Van Spaendonck-Zwarts, Circulation, 2010).
While the exact cause of PPCM is unknown, reference has been made to the possible involvement of various pathophysiological avenues e.g. infections, cardiotropic viruses, autoimunity or immune system dysfunction; inflammatory, metabolic and endocrine triggers, genetics, pre-eclampsia, which can produce an achievement, functional and anatomical cardiomyocytes and finally progressive dilation of the heart chambers with systolic dysfunction (BADEA, Ann Fr year Reanim, 2009, Van Spaendonck-Zwarts, Circulation, 2010).
Diagnosis
Diagnosis of cardiomyopathy of peripartum is by exclusion of other causes of heart failure. It rests on the combination of an array of clinical heart failure and left ventricular systolic dysfunction as evidenced in ultrasound or magnetic resonance imaging. The most frequent clinical symptoms include dyspnea, orthopnea, cough, edema of the lower limbs, ascites, palpitation, precordial pain, central or peripheral embolism, crackles, sounds of galloping, mitral and tricuspid insufficiency. One of the forms of presentation can be acute edema of the lung, cardiogenic shock and sometimes even a sudden death due to malignant
ventricular arrhythmia.
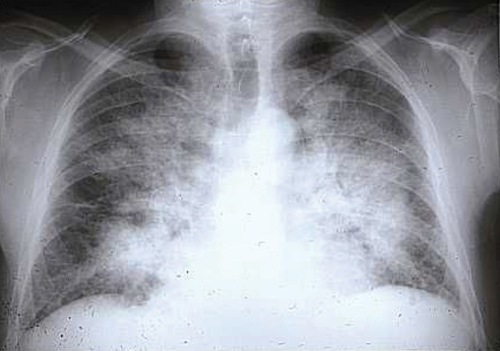
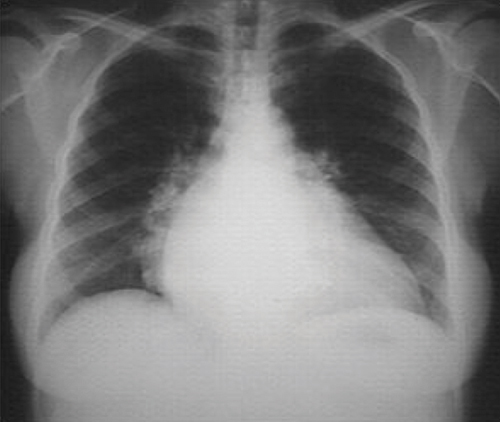
Seen in the chest x-ray, there are cardiomegaly and signs of pulmonary venous congestion with interstitial edema. Electrocardiagrams can also show disorders of ventricular repolarization, alterations in STEMI, left branch block, sinus tachycardia, disturbances of rhythm and other conditions of note.
 But the decisive consideration is the transthoracic ultrasound that will highlight the expansion / alteration of systolic left ventricular function, segmental contractility diameters of other cavities, valvular alterations and also assess the diastolic function of the left ventricle. Given the prothrombotic state connected with the pregnancy, the reduction in contractility, this echocardiography will seek to carefully search for the presence of thrombus intracavitary.
But the decisive consideration is the transthoracic ultrasound that will highlight the expansion / alteration of systolic left ventricular function, segmental contractility diameters of other cavities, valvular alterations and also assess the diastolic function of the left ventricle. Given the prothrombotic state connected with the pregnancy, the reduction in contractility, this echocardiography will seek to carefully search for the presence of thrombus intracavitary.
Other complementary examinations (blood chemistry and imaging) are very important because they offer additional items but also to help to assess the co-morbidity factors and to assess and establish differential diagnosis.
 Treatment
Treatment
The treatment is the same as any other form of acute systolic heart failure, pharmacological and the non-pharmacological. Converting enzyme inhibitors are contraindicated during the pregnancy but it is mentioned in post partum. Diuretics, beta-blockers following functional class, nitrates, and positive inotropics might merit a place in the treatment protocol. The introduction of anticoagulant should be considered in the case of systolic function less than 25%, because of the increased risk of embolism. Other treatment possibilities include: the use of anti-arrhythmics, pace pacemaker and, in the most severe cases, as a last resort, you can proceed with a heart transplant.
There is a full recovery of the systolic function in 50% of cases. Mortality is very high by 25-50%. Any subsequent pregnancy should be discouraged, especially in the case of persistent systolic dysfunction under treatment because recurrence is very common.
Cardiomyopathy is a serious disease in pregnant women or during the postpartum and it deserves timely, effective treatment to avoid serious complications.
References:
1. Bahloul M., Ben Ahmed MN., Laaroussi L., et al. Myocardiopathie du péripartum. Annales fr Anesth Réa, 2009; 28:44-60
2. Peripartum Cardiomyopathy: Review and Practice GuidelinesAm J Crit Care 2012; 21(2):89-98
3. Warnes CA. Pregnancy and heart disease. In: Bonow RO, MannDL, Zipes DP, Libby P, eds. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 82.
4. Ansari AA, Fett JD, Carraway RE, Mayne AE, Onlamoon N, Sundstrom JB. Autoinmune mechanisms as the basis for human peripartum cardiomyopathy. Clin Rev Allergy Inmunol 2002; 23 (3): 301-24.
5. Sliwa K, Fett J, Elkayam U. Peripartum cardiomyopathy. Lancet 2006; 368: 687-693.
6. Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J Heart Fail. Aug 2010;12(8):767-78










