Anthony Karabanow, MD
Tetanus is endemic in Haiti. According to WHO data, 16-119 cases have been reported annually since 2004. Immunization coverage in Haiti against tetanus is approximately 50%. Fatal cases of tetanus were observed in the aftermath of the Haitian earthquake.
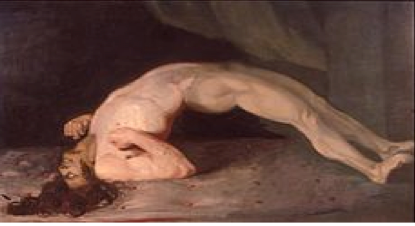
Tetanus is caused by Clostridium tetani which is found widely in soil as a spore (or inactive form.) When inoculated into wounds, this bacterium transforms into an active form and begins producing tetanus toxin. This toxin binds to nerve endings causing the classic symptoms associated with tetanus: increased muscle tone, painful spasms and autonomic instability (labile blood pressure, elevated heart rate, fever.) Tetanic spasms cause the most well known manifestatations of this disease: trismus (lockjaw), risus sardonicus (sarcastic smile) and opisthotonus (see picture below.)
Because Clostridium tetani is an anerobic bacterium (grows only in the absence of oxygen,) only certain wounds can allow this organism to germinate. Such tetanus prone wounds include: deep penetrating wounds, compound fractures, wounds with foreign bodies, wounds contaminated by soil, wounds with extensive tissue damage and burns.
 Generalized tetanus is the form most likely to be encountered. Localized and cephalic tetanus refer to tetanus occurring in a single limb or in the cranial nerves. These typically evolve into generalized tetanus. Neonatal tetanus results from umbilical stump infection or non-sterile delivery. This is characterized by: inability to suck, seizures, rigidity and spasms.
Generalized tetanus is the form most likely to be encountered. Localized and cephalic tetanus refer to tetanus occurring in a single limb or in the cranial nerves. These typically evolve into generalized tetanus. Neonatal tetanus results from umbilical stump infection or non-sterile delivery. This is characterized by: inability to suck, seizures, rigidity and spasms.
Tetanus is a clinical diagnosis made on the basis of a tetanus prone wound, inadequate vaccination and suggestive signs/symptoms.
There is no specific treatment for tetanus. Tetanus toxin binds irreversibly to nerve endings. These nerve endings must regenerate to end the clinical manifestations of tetanus. This process takes 4-6 weeks. In the interim, management consists of: wound care, antibiotics, toxin neutralization, spasm control and immunization against future disease.
Wound care: This requires aggressive surgical debridement of the wound to both remove the tetanus spores and the necrotic tissue necessary for their germination.
Antibiotics: By the time tetanus is diagnosed, tetanus toxin has already been produced and has bound to nerve endings. Thus antibiotics play a relatively minor role in therapy. They do kill residual bacteria and thus reduce the amount of available toxin.
Penicillin has been the traditional drug of choice but metronidazole is generally preferred. Given the possibility of mixed infection within the wound, it is suggested that ceftriaxone be used (1 gm IV/IM daily for 5-7 days.).
 Toxin neutralization: Only unbound toxin can be neutralized (i.e. that not bound already to nerve terminals.) This is accomplished by giving tetanus immunoglobulin via the intramuscular route (3000 – 6000 units.) Unlike the case of rabies, this does not need to be given at the wound site.
Toxin neutralization: Only unbound toxin can be neutralized (i.e. that not bound already to nerve terminals.) This is accomplished by giving tetanus immunoglobulin via the intramuscular route (3000 – 6000 units.) Unlike the case of rabies, this does not need to be given at the wound site.
Symptom control: Tetanic spasms are very painful and can be life threatening. Moreover, tetanus does not result in impaired consciousness – patients are very much awake and alert. At the very least, patients should be placed in a quiet room. This is because spasms are usually triggered by such stimuli as noise and touch. Benzodiazepines (Valium, Ativan, etc.) are the foundation of treatment for spasms. When these agents fail, the next step is to use paralytics and mechanical ventilation.
Autonomic instability (labile blood pressure, tachycardia, etc.) is best treated with intravenous magnesium. This is easily accessible from the obstetric unit where it is used to treat eclampsia. The doses are: loading dose of 40 mg/kg over 30 minutes followed by a continuous infusion of 2 gm/hr (for patients > 45 kg) or 1.5 gm/hr (for patients < 45 kg)1. Immunization: Suffering from tetanus does not grant immunization against future disease. Thus all patients with tetanus need to receive appropriate immunization. Since tetanus symptoms can last 4-6 weeks (the time necessary for nerve terminals to regenerate,) all care appropriate to a long term stay patient must be considered. This includes DVT prophylaxis, nutritional support, physical therapy and avoidance of skin breakdown. Neonatal tetanus has a case fatality rate of 10-60% and may result in long term neurologic deficits2. Non-neonatal tetanus has a case fatality rate of 8-50%2. Fatality rates are a better indication of the quality of available medical care rather than the severity of the disease. References: 1. Thwaites CL et al. Magnesium sulfate for the treatment of severe tetanus. Lancet 2006;368 (9545);1436. 2. Roper MH et al. Maternal and neonatal tetanus. Lancet 2007;370(9603):1947.









