In November 2012, CRUDEM and Hôpital Sacré Coeur staff engaged in a detailed strategic planning session and produced a five year strategic action plan with specific goals for hospital excellence. For maternal and newborn care they determined to: 1) look at the quality of services available to women and infants and 2) reduce intra-hospital maternal mortality by 75% and neonatal mortality rate by 25% in 2014.
In the years before the 2010 earthquake, Georgetown University Medical Center teams had visited the hospital. Our team’s overarching goals at the time were to assist the hospital in thinking about their overall quality of care and excellence in clinical training, particularly in the fields of women’s and newborn health. We conducted multiple teaching programs.
There were teaching weeks for traditional birth attendants (TBA), an American Life Support Obstetrics program (ALSO) which was geared for third world obstetric emergencies, Helping Babies Breathe (HBB), a low-tech NIH, American Academy of Pediatrics program called the S.T.A.B.L.E. program, another NIH program for hospital stabilization of newborns, and Neonatal Resuscitation Protocol (NRP) certification courses. To complement all these earlier didactic sessions and our Milot workshops, and to support the specific goals outlined in November 2012 Action Plan, we invited five staff members to come to Washington, D.C. in May 2014.
Hospital leadership was aware that in order to achieve the quality and safety goals, the staff would have to be trained in the concepts of safety and quality and then be prepared to bring these concepts back home in a ‘train the trainer’ model.Some examples would have to include: role playing the common emergencies they experience in Milot, particularly post partum hemorrhage (WHO statistics recognize it as a major preventable cause of maternal deaths). Another example would be to include proven medical crisis communication techniques learned from the training of military and civilian experiences.
There are simple, no cost, uncomplicated measures that could, for example, involve a short daily briefing of all medical staff at the beginning of the work day, called “huddle” — adapted for hospital use from a football team’s quarterback huddles.
After introducing the team to some of these concepts and exercises, we expected that they would adapt these low-cost, definitely low-tech measures, and them bring back to HSC and train their own staff.
Hôpital Sacré Coeur CEO Dr. Harold Prévil selected the team, which included: Winston Blaise, M.D. from the OB-GYN department, pediatrician Michele Hanna, M.D., nurse midwife Elise Belamour, obstetric nurse Jeanise Nicolas and pediatric nurse Aniola St. Juste. It was truly a multi-disciplinary team.
The team’s day began with early Sunday flights from Cap Haïtien to Port au Prince, to Miami, to Raleigh Durham and finally to Reagan National airport in Washington, D.C. Upon their midnight arrival in Washington, the team was greeted by Sister Mary Berchmans at the Visitation Monastery, located next to the Georgetown Medical campus.
Monday morning began with a coffee and bagel in Georgetown Hospital’s Pediatric conference room with the Georgetown faculty, CRUDEM board member Dr. Joseph Giere OB/GYN, neonatologist Dr. Deb Hoy, Elizabeth Robson CNM/NICU nurse specialist and Dr. Ranit Mishori, MHS Global Health/Family Medicine. All were old acquaintances of the Haitian visitors.
Dr. Kettie Louis arrived after an early morning flight from Boston where she currently teaches the USAID Masters program, preparing Haitian nurses to teach nursing education. During the day, Dr. Kettie presented French/Creole Powerpoint presentations on Interdisciplinary Communication, Patient Safety in Obstetrics and Hospital Communication Techniques. All these topics are recognized as basic tools to improve patient care and to import quality measures in American hospitals.In her follow-up workshops, Dr. Louis introduced the importance of team meetings to assess care. She stressed that the team should meet periodically. The team should review all care outcomes, both good and bad. Every team member must be empowered to speak freely. The final result could not be to assign blame, but instead to craft team consensus and arrive at “best practices” for Hôpital Sacré Coeur.
Dr. Kettie introduced “Root Cause Analysis” as another proven tool that should be used to aid problem solving in Milot.
She explained “Root Cause Analysis,” which meant asking multiple questions. It is looking for the “what happened” and “why did it happen” in a clinical situation. By reviewing maternal or neonatal mishaps, by discussing mortality and morbidity outcomes as a team, glitches could be identified and problems could be anticipated. She explained that as a result, the team must form a consensus protocol: a plan to follow and improve on performance. Dr. Louis asked the group for practical examples from their experience, and to then use those examples to problem solve in the group.One example they offered was how to effectively summon an emergency team when colleagues were scattered throughout the hospital compounds. How could their OR emergency response work if the person needed was unreachable or unable to come? Would the informal call system they used by sending notes or relying on their private phones to call for help be the best solution? What other better back-up plans could be in place that could be implemented realistically? What further thinking of work schedules or assigned duties or what training practice needed for new skills might be in order? For any progress in good medical care the group needed to think about how to problem solve in Milot directly with their colleagues.
Tuesday was another full day devoted to the Georgetown medical campus simulation laboratory.
Dr. Wendy Thorson, Ed. D., Director of Simulation Education and Research and Jessica Gordon, MSN, Manager of Medical Technologies, conducted the daylong seminar. They began with another discussion of team building and effective team communication.They reiterated the importance, even within a seasoned team, of emergency co-workers pausing often to call out to each other their actions so that all team members, even newcomers, could be integrated rapidly with the team veterans. “Emergencies needed to be practiced with simulations before and not during an event.” “Realistic simulation always helps,” was their mantra. They cited data to prove simulation practice for post partum hemorrhage emergencies or arrested labor practice has produced better patient outcomes.
They explained SBAR communication technique, which hospital nurses use daily. They rehearsed SBAR by having the team respond to the arrival at Hôpital Sacré Coeur of a pregnant woman in premature labor. Each team member had to respond as they progressed through the patient’s hospital entry for her premature delivery. By programming the obstetric manikin, “Noelle’s” lab to mimic vaginal delivery, Dr. Thomson supplied the role of the emergency patient. She programmed Noelle to challenge the team and showed how the non-mechanical pelvic model in Milot would accomplish all the simulation practice needed for effective training. Noelle was used for a couple more practice deliveries followed by a critique to nail down the important learning experiences.
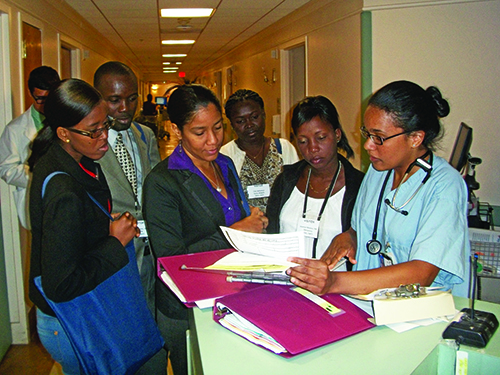
Wednesday.This was a third full day at Providence Hospital, operated by the Daughters of Charity. Training organizers chose this clinical site for the opportunity to review medical care in a large community hospital similar to Hôpital Sacré Coeur.
The day began with a pediatric and obstetric team “huddle.” A scheduled cesarean section was being readied when we arrived. The high risk NICU was planning to discharge their single patient. However, by shift end, several new admissions had occurred. The c-section time had to be reshuffled. Our visitors were able to observe unscripted Providence staff communication; how their brief team huddles worked during the day as new laboring patients were admitted, deliveries occurred, and as census climbed to eight NICU isolettes.
They were able to observe how good protocols, team training and staff communication could accommodate the changes even in an obstetric ward.
A Creole speaking resident in training, Tracy Casagnol led the group through the wards and explained how the work flow was organized. After a hospital cafeteria lunch, the group went to Providence Hospital’s staff training lab to again role-play normal delivery with Noelle. The Providence instructors tasked them to think of how they could use the Milot pelvic model and how to role play. The Haitian team used simulation exercises for emergency bleeding and other emergencies. Dr. Hanna and nurse Aniola awaited the routine delivery and prepared to receive baby ”Hal.” Although Hal could be programmed for a routine uncomplicated delivery, the simulation instructors added several delivery room problems. Before the end of today’s training session, our Milot pediatric team had to deal with a distressed, unresponsive limp Baby Hal with oxygen deprivation and a low temperature. Complications in labor were programmed into Noelle as well.
Training like this is important. These Providence Hospital simulations reflected all too frequent real life Haiti. They were chosen and repeated Tuesday, Wednesday and Thursday for these very reasons.
Thursday.
The venue for Thursday morning was Medstar/ Georgetown’s midtown Simulation Center (SITEL) on Connecticut Avenue, several blocks from the National Zoo. The Center is used by all the Mid-Atlantic region hospitals for staff training and certification. (American hospitals now require all staff to train and demonstrate their job proficiency skills periodically.) Our purpose here was to train the trainers and prepare them to be able to use the pelvic and baby simulation models we have stored in Milot, which we used in our past training programs.
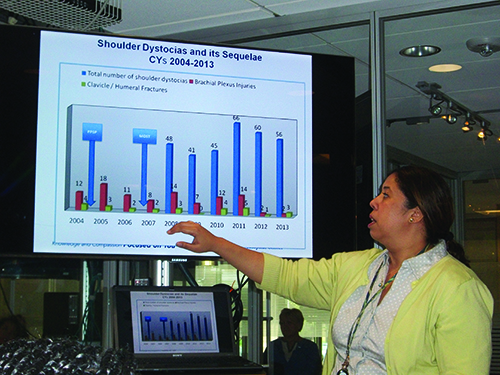
She presented research statistics to prove to the Milot team that simulation practice produces improved patient care and safety.
The Center has setups to practice skills in blood drawing, placing tubes, inserting infant airways, etc. One tool unique to the Center is a virtual reality surgical skill trainer. This tool is a suitcase sized model connected to a computer. It enables the learner to practice hand-eye surgical skill coordination. Medical scenarios actually replicate immediate visible results on the computer screen. As the student manipulates surgical instruments to surgically cut, suture and cauterize, he or she can see what is happening — tissues are separated, and vessels bleed.
The center donated three complete surgical skills training practice kits that the group brought back to Hôpital Sacré Coeur. Each of the kits contained instruments and web cam with practice sets. Once connected to a computer, an operator should be able to master maneuvers needed in the OR or in the NICU.After three and a half intensive days the team asked to have a break. They all wanted to see the White House. Elise wanted to SKYPE her son a happy birthday and Michele looked for model trucks for her young sons. They were not too tired for a brief side detour to a Target store on the route to the White House. On arrival, while walking around the gates in the Washington heat, they mingled with tourists from China, Mongolia, European Georgia and the state of Georgia. They went over to the Organization of American States, then on to the Smithsonian to see the Hope Diamond, the Natural History Museum’s Rotunda Elephant and the First Ladies’ dresses.
Although the current president was not available, they stopped at the National Mall for Presidents Thomas Jefferson, Franklin Roosevelt and Abraham Lincoln, as well as a tour to see The Rev. Dr. Martin Luther King, Jr.’s memorial.
Friday was the first day to sleep until eight. Beth Robson “midwifed” a short break with the ladies. They went for a morning walk through the mega malls at Tyson’s Corner in Virginia. A suitcase broke. It had been stuffed with a supply of Costco protein bars Sister Anne uses for the pediatric patients hospitalized for malnourishment. Would that all the problems were so easy! Most American basements come with stored suitcases nowadays.Friday afternoon was back to work at Georgetown for a wrap-up session of the week’s work. Dr. Deb Hoy came armed with a Powerpoint she had prepared.
Everyone agreed, the five colleagues from Milot could return empowered to help their colleagues back home. We hope they will succeed!
Joseph Giere, M.D. is a Maryland based OB-GYN and CRUDEM Board member who regularly volunteers at HSC.