Anthony Karabanow, MD
Diarrhea is defined as the passage of 3 loose stools within 24 hours. It is a leading cause of child mortality in the developing world. The approach to acute diarrhea (i.e. less than 14 days) will be discussed below. National surveillance data in Haiti regarding specific diarrheal pathogens is not available. What follows is a general discussion regarding acute diarrhea in the developing world. Care standards are according to the WHO literature. Of note, Hopital Sacre Coeur does not have the capacity to perform stool culture at this time.
Diarrhea is divided into watery and bloody forms:
WATERY DIARRHEA:
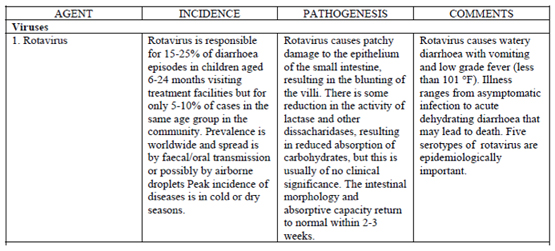
In infants and young children, the most likely pathogen is rotavirus. In older children and adults, enterotoxigenic E.Coli is the leading cause. Under outbreak situations when patients are experiencing large volumes of rice water stool, cholera needs to be considered. The diagnosis and treatment of cholera are discussed separately. For watery diarrhea, the principle treatment modality is hydration. Antibiotics are seldom necessary.
BLOODY DIARRHEA:
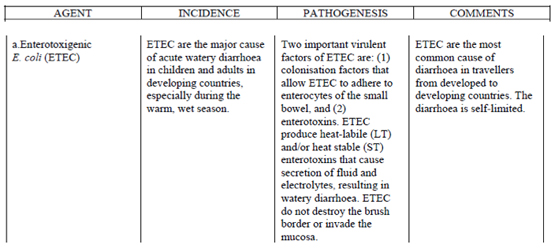
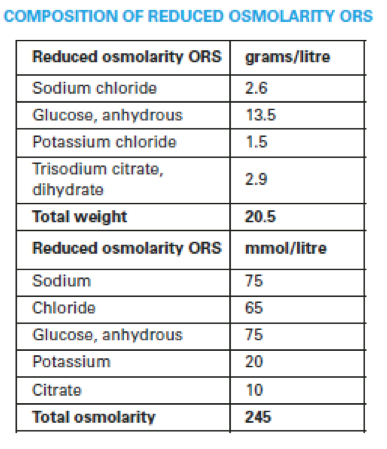
Dysentery refers to a syndrome of bloody diarrhea accompanied by fever. The most common cause would be Shigella. Dehydration is rarely of concern due to the small volume of stools. However, due to the invasive nature of this infection, antibiotics are usually recommended:
The use of TMP-SMX and amoxicillin is strongly discouraged due to widespread resistance to these agents.
If the diarrhea fails to respond to the above empiric therapy, treat for presumptive resistant Shigella with a different agent (e.g. ceftriaxone). If the diarrhea still fails to resolve, treat with metronidazole to cover Entamoeba histolytica:
VITAMIN SUPPLEMENTATION:
In children, zinc supplementation reduces the frequency and duration of an episode of acute diarrhea. A 10-14 day course reduces the incidence of diarrhea in the following 2-3 months. The dose is 20 mg daily for 10-14 days (10 mg in those 6 months or younger).
ANTIDIARRHEAL AGENTS:
These are best avoided in cases of infectious diarrhea. These agents may cause paralytic ileus or prolong infection by delaying the elimination of the causative organism. They should never be given to children <5 years of age.
ORAL REHYDRATION SOLUTION (ORS):
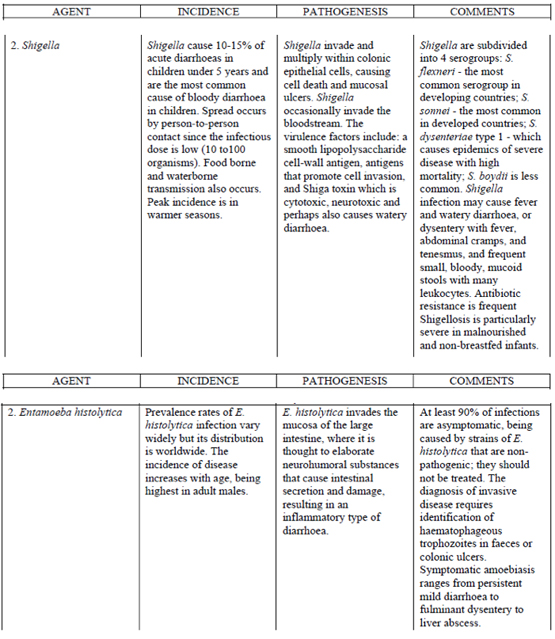
Oral rehydration is the preferred means of fluid resuscitation in the developing world. It is both highly efficacious and cost effective. Intravenous fluid resuscitation should NOT be used routinely unless indicated below. The current ORS in distribution is the so-called reduced osmolarity ORS. This has been shown to reduce diarrhea and vomiting compared to regular ORS. Its composition is as follows:
WHO RESUSCITATION STRATEGY:
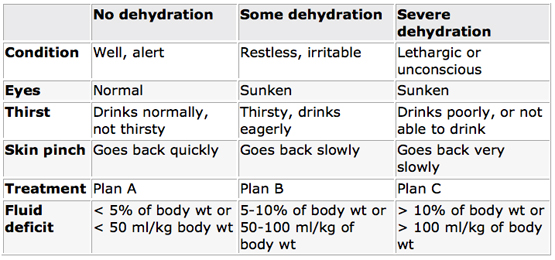
The first step in resuscitation is to determine the degree of dehydration.
PLAN A: MILD DEHYDRATION
Those with no signs of dehydration need extra fluid and salt to replace their losses of water and electrolytes due to diarrhea. The preferred rehydration fluid is ORS. Plain water should also be given. Commercial carbonated beverages, fruit juices, sweetened tea, coffee, medicinal tea should be avoided. The appropriate amounts of fluid are as follows:
• Give as much fluid as the child wants until the diarrhea stops
• Children < 2 years of age: 50-100 ml of fluid
• Children 2-10 years: 100-200 ml
• Older children and adults: As much as they want
Diet should be continued during diarrhea and increased afterwards. Breastfeeding should always be continued.
PLAN B: MODERATE DEHYDRATION
For moderate dehydration, the preferred rehydration strategy is via ORS. The following amounts of ORS should be administered within the first 4 hours:
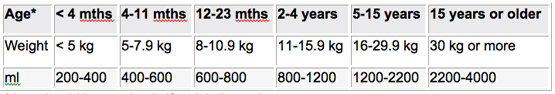
*Age should be used only if weight is not known.
The approximate amount of ORS required (in ml) can also be calculated by multiplying the patient’s weight in kg by 75. If more ORS is required, more may be provided. Except for breast milk, food should not be given during the initial 4 hour rehydration period. However, those continued on treatment Plan B longer than 4 hours should be given some food every 3-4 hours as in Plan A. After 4 hours, the patient should be reassessed and further treatment provided based on the degree of dehydration.
PLAN C: SEVERE DEHYDRATION
The preferred treatment for severe dehydration is rapid intravenous rehydration with Ringer’s lactate or normal saline solution.
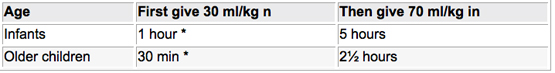
* Repeat once if pulses are weak or not detectable.
The patient should be reassessed every 1-2 hours. If hydration is not improving, the intravenous infusion rate should be increased. After the completion of intravenous fluid resuscitation, the patient should be reassessed and the appropriate treatment (Plan A, B or C) chosen. If intravenous therapy is not available, then ORS via nasogastric tube or orally at 20 ml/kg/hour for 6 hours (total of 120/kg) should be given.
PREVENTION:
Diarrhea is transmitted by the fecal-oral route. Thus interruption of transmission relies on:
• The consumption of safe food and water
• Handwashing
• The WHO has issued a call for the inclusion of the rotavirus vaccine in all national vaccination programs.
END NOTE:
Diarrhea may be part of the presentations of such disorders as HIV, influenza, malaria, pneumonia, meningitis and UTI. These diagnoses need to be considered under the appropriate circumstances.
References:
1. Treatment of Diarrhea WHO Guidelines 2005.