This article is designed to introduce the health care practitioner to the diagnosis and treatment of TB in Haiti based on available resources at Hôpital Sacré Coeur and according to Haitian national TB standards. Drug resistant TB is not covered. TB occurring in the HIV patient is addressed in the article entitled “HIV IN HAITI.”
EPIDEMIOLOGY:
According to the USAID website:
“Haiti has the highest per capita tuberculosis (TB) burden in the Latin America and Caribbean region. After HIV/AIDS, TB is the country’s greatest infectious cause of mortality in both youth and adults (6,814 deaths in 2007.) Haiti is among the eight priority countries identified by the Pan American Health Organization for TB control in the region. According to the World Health Organization’s (WHO’s) 2009 Global Tuberculosis Control Report, Haiti had an estimated 29,333 new TB cases in 2007.
A major problem in combating TB is that co-infection with HIV can run as high as 30 percent in some urban areas.Strong stigma and cultural barriers attached to TB also interfere with case detection and adherence to treatment. Multidrug-resistant (MDR) TB has increased from 1.4 percent in 2004 to 1.8 percent in 2007.”
PATHOPHYSIOLOGY:
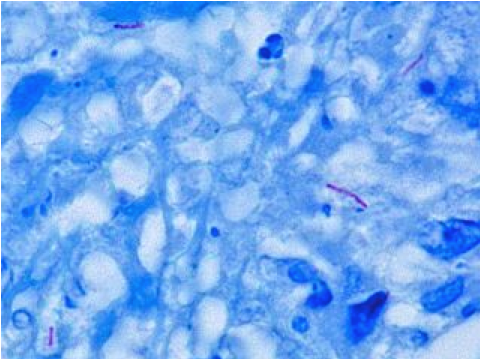
Tuberculosis is caused by the bacterium Mycobacterium tuberculosis. Its cell wall structure confers a resistance to destaining by acid alcohols after being stained by certain aniline dyes (hence the term acid fast bacillus or AFB.) Thus the detection of AFB in tissue samples by microscopy is the most common means of detecting TB.
TB is transmitted from person to person via small droplets (several microns in diameter) produced by coughing. After the inhalation of mycobacterium tuberculosis bacilli, there are a number of possible outcomes:
1. The bacilli may be destroyed by the immune system.
2. The bacilli may be contained (but not destroyed) by the immune system. This typically occurs after a period of bacteremia. The bacilli are capable of causing disease at a later date should the immune system falter in its containment. This may occur due to advancing age, HIV, diabetes or the administration of immunosuppressive medications (such as prednisone.) Such disease is termed reactivation TB.
3. The bacilli may overcome the immune system and cause immediate disease. This is termed primary TB.
PULMONARY TB:
Pulmonary TB should be suspected in anyone who presents with fever, chills, night sweats and cough (possibly blood tinged) of greater than 2 weeks duration. Such patients should undergo evaluation by chest x-ray and serial sputum collection for AFB staining. Three sputum samples are to be submitted at least 8 hours apart with at least one early morning sample. Unfortunately no TB culture is possible at Hôpital Sacré Coeur. TB culture is more sensitive than AFB staining and allows for the determination of drug susceptibility. If such testing is deemed necessary, samples will need to be sent to Port au Prince.
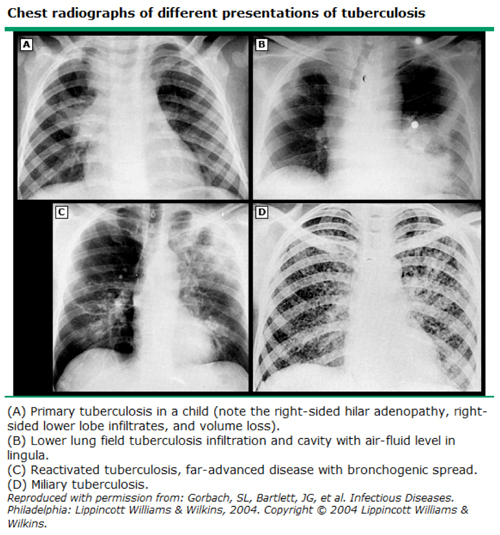
In primary TB, the most common radiographic abnormalities are hilar adenopathy, pleural effusions, and infiltrates (right sided and peri-hilar.) The classic chest x-ray in reactivation TB demonstrates focal air space disease in the upper lobe.
Miliary TB refers to uncontrolled, widely disseminated TB. The term “miliary” refers to the appearance of the chest x-ray as being full of millet seeds.The treatment for miliary TB is the same as for pulmonary TB.
It is important to note that a positive PPD indicates only prior exposure to TB. It is typically positive in those with active TB. However, it may be negative in those with advanced TB and in those with concurrent HIV. The diagnosis of TB requires the identification of mycobacterium in a clinical sample.
EXTRAPULMONARY TB:
Although commonly thought of as a respiratory disease, TB can affect virtually any organ system. We will address 2 of the most common extra-pulmonary manifestations – spinal TB and TB lymphadenitis and TB.
 SPINAL TB (Pott’s disease):
SPINAL TB (Pott’s disease):
Spinal TB (or Pott’s disease) typically affects the lumbar and lower thoracic regions. In highly endemic areas, spinal TB usually occurs in the young as a consequence of primary TB infection. The vertebral bodies are especially vulnerable to TB infectious due to their relatively high blood flow. TB of the spine is a typically indolent disease manifesting as increasingly severe, localized spinal pain and associated muscular spasm over a period of weeks to months. Patients often demonstrate a characteristic gait – walking gingerly and erect to minimize pain. The typical constitutional symptoms of TB (weight loss, night sweats etc) are only present in a minority of patients. The most important complication of spinal TB is that of abscess formation which may cause cord compression. Due to delays in seeking medical care, this is a common presentation in the developing world.
The diagnosis of spinal TB relies on obtaining a biopsy specimen for AFB staining. Unfortunately, this is rarely possible. Typically, the diagnosis is suggested by a positive PPD and a suggestive spinal x-ray.
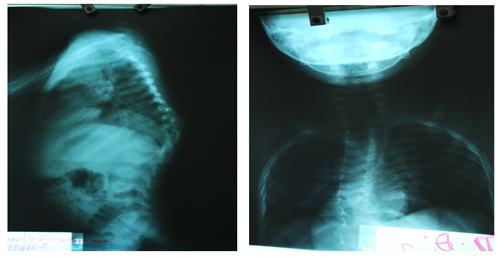
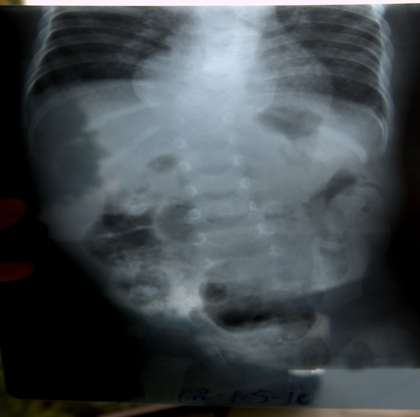
No x-ray findings are pathognomonic for TB. Early findings include soft tissue swelling, osteopenia and bone destruction with relative preservation of disc space3. Late findings include structural collapse, sclerotic changes and soft tissue calcification3. Ultimately a Gibbus deformity may be seen. This is a step kyphosis which results from progressive disc space collapse with anterior wedging and angulation.
Spinal abscess formation is suggested on x-ray by the presence of probable bony TB disease and flaring of the para-spinal musculature (note the “double heart border” below.)
 The treatment regimen for spinal TB is identical to that for pulmonary TB. Surgery may be required for spinal stabilization, abscess drainage or spinal decompression due to neurologic deficits. A spine surgeon with experience in TB needs to be consulted in these cases.
The treatment regimen for spinal TB is identical to that for pulmonary TB. Surgery may be required for spinal stabilization, abscess drainage or spinal decompression due to neurologic deficits. A spine surgeon with experience in TB needs to be consulted in these cases.
TB LYMPHADENITIS (SCROFULA):
TB lymphadenitis (or scrofula) is usually the result of the reactivation of latent disease. It most commonly involves the cervical nodes. Physical examination typically reveals a firm mass fixed to underlying structures.
The diagnosis is made by fine needle aspiration and AFB staining. The treatment is the same as that for pulmonary TB.
TREATMENT PROTOCOLS FOR ADULTS:
The following abbreviations are used for TB meds in Haiti and in the WHO literature:
H = INH, R = Rifampin, E = EMB (ethambutol) and Z = PZA (pyrazinamide)
S = Streptomycin
In Haiti, TB medications come in fixed dose combination pills and are given on a daily basis throughout the treatment course:
RHEZ = 75 mg INH, 150 mg Rifampin, 400 mg Pyrazinamide , 275 mg Ethambutol
RH = 75 mg INH, 150 mg Rifampin
RHE = 75 mg INH, 150 mg Rifampin, 275 mg EMB
The doses of the TB meds are (for daily administration):
INH 5 mg/kg (300 mg max) Rifampin 10 mg/kg (600 mg max)
PZA 25 mg/kg EMB 15 mg/kg STREPTOMYCIN 15 mg/kg IM
 According to Haitian TB treatment standards, patients are divided into 3 categories:
According to Haitian TB treatment standards, patients are divided into 3 categories:
1) Category 1: Patients never before treated for TB
2) Category 2:
• Relapsing patients – i.e. those with a new diagnosis of active TB after completing a prior course of TB meds.
• Treatment failures – a patient with AFB positive sputum after 5 months or more of anti-TB drug treatment.
• Treatment interruption – a patient with a 2 month or greater period of treatment interruption and AFB positive sputum
3) Category 3: Resistant TB
These categories are treated as follows:
1) Category 1: 2 months RHEZ then 4 months 4RH
2) Category 2: 2 months SRHEZ then 1 month RHEZ then 5 months RHE
3) Category 3: This will not be discussed here. These patients require referral to a specialty TB facility.
All patients receiving INH should also receive pyridoxine 25 mg daily to prevent peripheral neuropathy.
FOLLOW UP:
Patients needed to be followed up at regular intervals (typically monthly) to determine their response to therapy and to elicit adverse drug reactions. The patient’s weight should be followed regularly. All TB medications should be given via DOT (directly observed treatment) to maximize compliance and to reduce the rates of drug resistance.
New cases of TB have AFB staining of their sputum after 2, 5 and 6 months of treatment. If the 2 month AFB is positive, the initiation phase is prolonged another month and another AFB is performed at the 3 month mark. If the 3 month AFB is still positive, drug sensitivity testing needs to be performed. A positive AFB at the 5 or 6 month mark also requires drug sensitivity testing.
In cases of TB retreatment, AFB staining is performed after 3, 5 and 8 months of treatment. If the 3 month test is positive, the intermediate treatment phase is prolonged another month and drug sensitivity testing needs to be performed. A positive AFB at the 5 or 8 month mark also requires drug sensitivity testing.
With AFB negative TB cases (i.e. presumptive TB), a follow up AFB is performed at the 2 month mark only in those patients who are still symptomatic. In those patients with extra pulmonary TB, no follow-up AFB results are necessary. These cases are followed clinically. Weight gain is a reassuring sign.
TB INFECTION CONTROL:
Patients with untreated TB – especially when their sputum is AFB positive – are to be considered infectious. However, AFB negative patients can still transmit the disease. Extra pulmonary TB is not contagious.
Patients with pulmonary TB should ideally be managed in an outpatient setting (preferably at home.) Bringing these patients into the hospital setting (or clinic) risks the transmission of this disease to others (both patients and care providers.) Patients who are admitted to the hospital should be subject to the following infection control protocols:
1) The patient should wear a surgical mask. These masks are sufficient to prevent cough induced TB from becoming aerosolized. If surgical masks are unavailable, patients need to be instructed on cough etiquette.
2) TB patients should be isolated to a single room or rooms specially designated for such patients.
3) The TB rooms should be well ventilated to further reduce the concentration of airborne TB particles. This means open windows and fans.
4) Health care providers working on a TB ward should be provided with N95 masks if possible.
Patients are typically considered non-infectious when the patient has received 2 weeks of effective TB therapy and are improving clinically.
End note:
Given the high rates of HIV and TB co infection, all patients with documented TB need to be tested for HIV.
References:
1) Mohapatra PR, “Tuberculous lymphadenitis,” JAPI, 2009 Vol. 57: 585-590.
2) MANUEL DE NORMES DU PROGRAMME NATIONAL DE LUTTE CONTRE LA TUBERCULOSE 2010.
3) UpToDate
4) WHO TB Treatment Guidelines 2010.
5) WHO TB Infection Control Guidelines 2009.
6) USAID Haiti website