Typhoid fever is one of the classic tropical illnesses. Although largely forgotten in the developed world, it remains endemic in Haiti. However, there is no reliable data on its incidence. There have been anecdotal reports of past outbreaks but no published reports.
Typhoid disease refers to disease caused by the bacteria Salmonella enterica serotype Typhi (formerly Salmonella typhi.) A similar disease is caused by Salmonella paratyphi (paratyphoid fever.) These organisms are shed in the urine and stool of infected individuals and may subsequently contaminate food and water.
After ingestion, the bacteria invade the mucosa of the small intestine and take up residence in the lymphoid tissue. After an incubation period of 7-14 days, they are ultimately released into the bloodstream and disseminate widely to such sites as the liver, spleen, bone marrow and gallbladder. This coincides with the onset of clinical disease.
Classical reports of untreated typhoid fever describe the disease as occurring in stages.
1) Week 1: Patients usually present with fever, chills, myalgias, a dull frontal headache, dry cough and diffuse abdominal discomfort. The fever is classically “stepwise” – a rising temperature over the course of the day that drops by the following morning. A relative bradycardia or pulse-temperature dissociation is often reported. This means that the heart rate is relatively low given the degree of fever.
2) Week 2: The fever plateaus at 103-104 degrees (39-40 degrees). Abdominal pain increases and abdominal distention occurs. Adults often experience constipation. But in children and those with HIV, diarrhea is more common. The diarrhea is often likened to pea soup – foul swelling, green/yellow liquid. Rose spots may develop on the skin. These are crops of flat, salmon colored, blanching spots 2-4 mm in diameter on the chest and abdomen. These are unlikely to be seen in dark skinned individuals.
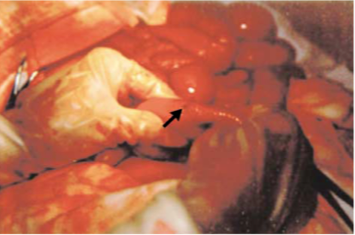
3) Week 3: The most severe symptoms occur at this time. These include sepsis, intestinal bleeding and intestinal perforation. A typhoid state of apathy is often noted. The intestinal bleeding and perforation result from inflammation of Peyer’s patches. These are lymphoid tissue which is found in the distal small bowel (the terminal ileum.) They are responsible for immune surveillance of the intestinal lumen. Their inflammation (and resulting bowel narrowing) also explains the phenomenon of constipation in typhoid.
4) Week 4: If the patient survives, recovery begins at this time.
 However, in the majority of patients, typhoid is a mild, non-specific, febrile illness which resolves either without treatment or which can be treated on an out-patient basis.
However, in the majority of patients, typhoid is a mild, non-specific, febrile illness which resolves either without treatment or which can be treated on an out-patient basis.
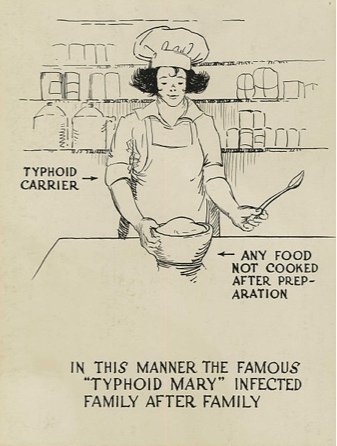
Relapse occurs in 5-10% of patients. The relapse is usually milder than the original disease and the organism usually has the same antibiotic susceptibility pattern as the original pathogen. Up to 5% of patients become long term carriers of the disease. These patients have no symptoms but represent an important reservoir of infection. “Typhoid Mary” was the most famous historical chronic typhoid carrier. She was a cook in early 20th century New York who spread the disease to many. Ultimately, she was incarcerated by the Public Health Service.
 Diagnosis is difficult in the developing world. The combination of fever and abdominal pain often prompts consideration of typhoid. However, this combination of symptoms is far from diagnostic. The best diagnostic test is blood culture. Unfortunately, this is not commonly available. An older test is in use called the Widal test. This test is not recommended. It measures serum antibodies to typhoid. Unfortunately, it cannot distinguish between past and current infection. This is particularly problematic is areas where past infections are common.
Diagnosis is difficult in the developing world. The combination of fever and abdominal pain often prompts consideration of typhoid. However, this combination of symptoms is far from diagnostic. The best diagnostic test is blood culture. Unfortunately, this is not commonly available. An older test is in use called the Widal test. This test is not recommended. It measures serum antibodies to typhoid. Unfortunately, it cannot distinguish between past and current infection. This is particularly problematic is areas where past infections are common.
Treatment is complicated by the development of antibiotic resistance. Older agents such as Bactrim, amoxicillin and chloramphenicol are no longer effective. The treatment of choice is currently ceftriaxone 2 gram IV daily or cipro 500 mg bid. The duration of treatment is 7-14 days depending on disease severity. In severe disease, steroids may be added (dexamethasone 3 mg/kg loading followed by 1mg/kg every 6 hours x 8 doses.) Severe typhoid fever represents one of the few bacterial infections in which steroid therapy may be indicated. Intestinal perforation requires prompt surgical intervention. Antibiotic coverage should also be broadened to cover bowel flora.
Relapsing typhoid fever is treated with another course of antibiotics. Asymptomatic carriers of typhoid are usually successfully treated with a prolonged course of antibiotics (eg cipro 500 mg PO BID x 2-4 weeks.) At times, the gallbladder (gallstones can harbor salmonella) must be removed.
The key to prevention is the consumption of clean food and water. For travelers to Haiti, vaccination is recommended. The oral vaccine last 5 years, the injection form 2 years. However, protection is far from complete (50-80%). Travelers are reminded of the mantra “Boil it, peel it, cook it or forget it.” Under outbreak situations, the primary control measure is drinking water chlorination. Another possible intervention is mass vaccination.
References:
1. Parry MP et al. Typhoid fever. N Engl J Med 2002; 1770-1781.